Most mothers experience the “baby blues,” which affect around 70-80% of new mothers for around a few weeks and then resolve. Postpartum depression is longer lasting and more severe and affects around 10% of new mothers, with frequent crying, fatigue, feelings of guilt and anxiety, and inability to care for the baby or yourself, according to the Cleveland Clinic. You can also feel “numb to the world”, have mood swings, feel hopeless, feel easily frustrated, or have feelings of anger. There are several other types of PPD including postpartum anxiety, postpartum OCD, postpartum PTSD (traumatic birth), and even postpartum psychosis.
Most risk factors for postpartum depression focus solely on maternal factors: dropping hormone levels of estrogen and progesterone after birth, a history of depression, sleep deprivation, lack of support from a partner/family/friends, unplanned pregnancy, teen pregnancy, and substance abuse issues. If any of those apply in your situation, as much as it depends on you, seek help for those specific issues. For example, if you are sleep deprived (and what new parent isn’t?), attempt to get more sleep as best you can, find support or a support group, and seek professional help and medications if necessary. These all certainly help a tremendous amount.
However, not much attention is given to infant factors that can complicate the “4th trimester” with poor breastfeeding or bottle-feeding, or babies who are colicky, fussy, gassy, and frequently spitting up. For many moms, the birth did not go according to plan, and then sometimes feeding doesn’t go according to plan either! The baby can’t latch, or when they do it’s terribly painful (7/10 pain is seen at our office daily, and last week one mom said 12/10 pain!). These symptoms are sadly common, but not normal. Often, not much support is given except “wait it out”, or band-aids that don’t address the root cause of the feeding difficulties. In our experience, treating a tongue-tie and helping with infant feeding is a significant non-pharmacologic intervention that can help with postpartum stresses, and we see many struggling moms feeling more confident and in a better emotional state at their 1-week follow-up. It was also confirmed in Dr. Ghaheri’s studies (here and here) reporting increased maternal self-confidence scores with breastfeeding after tongue- and lip-tie release.
These babies are given labels like “he’s a difficult baby” or “she’s just colicky” or “he’s just a GI baby,” meanwhile the parents and even the whole family are struggling because they are trying to feed a baby who spits everything up, is frustrated at the breast, or if bottle-feeding, falls asleep quickly and never finishes the bottle. Often, the reason the baby is crying or colicky is as simple as hunger (they’re not feeding well), and/or they are full of gas and uncomfortable. Also, just because a baby is gaining weight does not mean everything is ok. That’s setting a low bar: survival. We should be aiming much higher to help baby and mother (and father and siblings!) thrive.
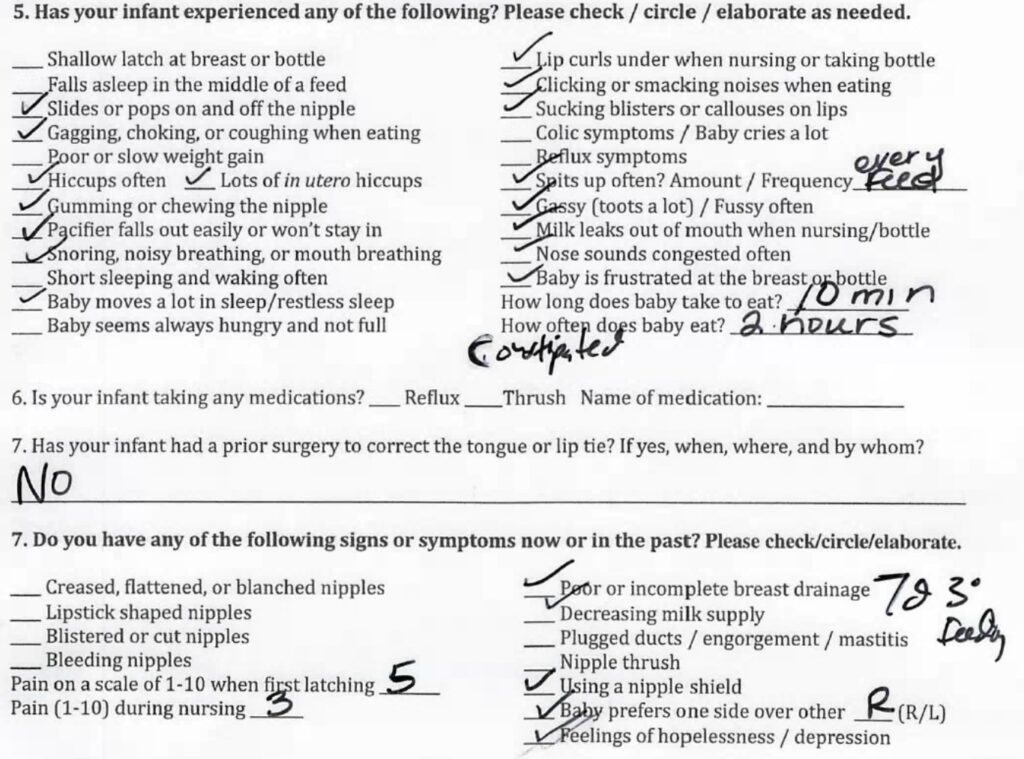
Here is a typical intake form from our office that we see multiple times a day (this one is from yesterday). Each of these checkmarks is an issue the family is struggling with and often is related to tongue-tie and lip-tie issues. Notice the check at the bottom for feelings of hopelessness or depression. Anyone working with new moms needs to ask about how they are doing emotionally, as it is certainly relevant.
Here’s where tongue-tie and lip-tie treatment can help. If we can help the baby get a deeper latch by releasing tissue under the tongue that is restricted with a simple procedure, and help them get a better seal at the breast or bottle by releasing a restrictive lip-tie, then we typically see resolution in many of those issues. Often we see one better feed (or more) the first day. For most moms, this equates to a “light at the end of the tunnel.” They have been trying to figure out what is wrong and perhaps have been dismissed, particularly if the tongue tie was not very obvious, as tongue-ties that are not to-the-tip are not picked up easily. Once the baby is eating better, they can start on the path of healing – physically, emotionally, spiritually, and mentally. When symptoms improve, moms realize they’re “not crazy”; they feel validated and in a better emotional state.
We do hear people almost daily say “this is my Hail Mary” or this is my last hope for getting my baby to breastfeed. They have tried everything and are at the end of their rope. We never shame mothers over not breastfeeding or any other issue, and we need to take care as a society to not pressure moms too much on this topic. But we do need to offer thoughtful assistance with these common infant issues and encourage providers to look for a potential deeper cause for infant feeding struggles. With tongue- and lip-ties being present in around 25% (some would say even higher) of babies, this is a very common issue that is often overlooked or dismissed. And we could help countless women who desire to breastfeed but find it difficult. Looking at the intake form above, you can see the common symptoms that are related to tongue- and lip-ties (and notice that baby was gaining weight well but still struggling). Here’s a follow-up form also from yesterday of a baby treated seven days before that mom is now feeling more confident and in a better emotional state. It’s not hard to imagine that if the baby is feeding better, spitting up less, sleeping better, and nursing is less painful for mom, it can help with all kinds of issues and stresses new families face.
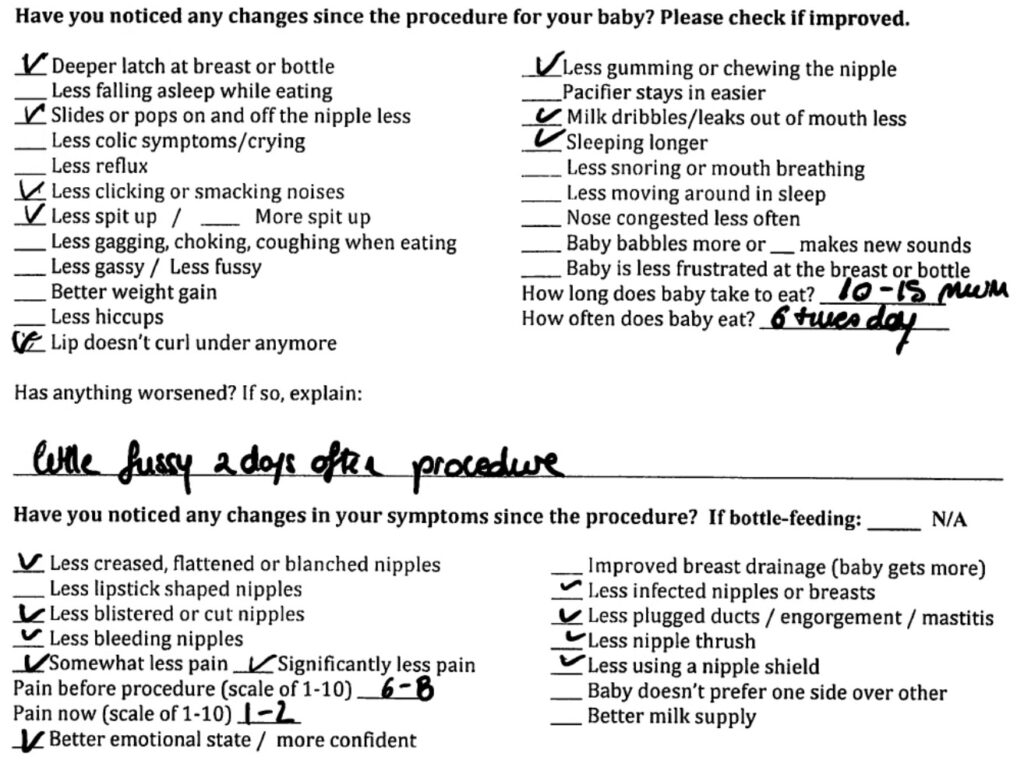
However, it’s not uncommon for a tongue-tie release to make things more difficult temporarily before it gets better. If the baby does not receive proper pain control (Tylenol, Motrin, etc.), then they may not want to eat right away. Also, not all laser releases are the same, and when we switched from the diode laser to the CO2 laser, we noticed a big decrease in infant pain both during and after the release. If a complete, high-quality release is done, typically a better outcome is achieved. A lactation consultant, or IBCLC, is critical as they support the mom before and after release, and are a resource and advocate for postpartum care and nursing struggles. Also, not having bodywork (chiropractor, CST, etc.) before the release means the baby is likely more in the fight-or-flight response, rather than rest-and-digest, and babies will have a harder time recovering. Lastly, the earlier the treatment is done, the better; a 1-week old baby will typically improve faster than a 1-month old baby, etc.
So what should you do? First, if you feel any thoughts of harming yourself or your baby, feel depressed most of the day, feel anxious, guilty, hopeless, or have lost enjoyment in everyday life, contact your healthcare provider right away. It might be the baby blues, but could just as easily be something more serious, like postpartum depression. If your infant is struggling to feed, making it feel like it’s a full-time job, you’re anxious about them getting enough milk, they’re spitting up constantly, not sleeping, and you don’t know what to do, there is likely something deeper going on. There is probably a reason why the infant (and you and Dad) are struggling. Get them evaluated for a lip- or tongue-tie by someone who treats tongue-ties routinely, as very often it’s involved as part of the problem. Send us a message, or call us at 205-419-4333 and we’d love to help. Hang in there; it will get better soon!
